의료진, 진료과/클리닉/전문센터, 질환정보, 자주하는질문, 병원소식이 통합검색 됩니다.
Our earnest steps forward to the core
essence go to the future.
- Doctors at a Glance
- Medical
Depts
MizMedi’s specialized medical
staff is always ready to help you.
- Location
- Phone Numbers
- Facilities
- Medical Services
MizMedi is equipped with the customer-
friendly facilities to provide the diverse
top-quality medical services.
MizMedi is dedicated to protecting
both your health and healthy life.
Having succeeded in the first in-vitro fertilization as a private hospital in 1987 and first Cryoperservation of human embryos in Asia in 1988, MizMedi’s iDream Clinic provides the top-quality infertility treatment service to bring the joy of pregnancy and delivery to those who are suffering from infertility.

-
High success rate of pregnancy
Highly experienced specialists appropriately employ artificial/in-vitro fertilization techniques, and laparoscopy and hysteroscopy to raise the success rates of pregnancy. An in response to the surging rates of male subfertility, the center closely works with the specialists of urology.
-
Leader in the field of subfertility
MizMedi Hospital was the nation first hospital to obtain the ISO accreditation in the field of subfertility treatment, standardizing the service system and managing the eggs/sperm/fertilized eggs in a systematic way, and, now as the leader in the field of subfertility, the hospital is focusing on distributing its proprietary techniques with continued research and development efforts.
-
Customized treatment service
MizMedi Hospital was the nation’s first hospital to obtain the ISO accreditation in the field of subfertility treatment, standardizing the service system and managing the eggs/sperm/fertilized eggs in a systematic way, and, now as the leader in the field of subfertility, the hospital is focusing on distributing its proprietary techniques with continued research and development efforts.
-
Most advanced embryo cultivation room
The entire spaces in the egg-collection room and embryo cultivation room are equipped with the special filtering equipment to block even the finest dust from entering the spaces and are also equipped with the embryo-cultivating incubators that use specially mixed gases to further raise the rates of pregnancy.
-
Cozy patients’ waiting room
The space utilizes natural lighting to the maximum to provide a cozy atmosphere for those who wait for diagnostic and treatment services.
Fields of Service
- Polycystic Ovary Syndrome/
Ovulation Disorder - Ovarian Dysfunction
- Male Infertility/Sperm Bank
- Artificial Insemination
- In-Vitro Fertilization
- Selection of Best Embryo
- Creating the Optimum
Condition for Implantation - Recurrent Miscarriage/
Recurrent Implantation Failure - Preimplantation Genetic Diagnosis
- Fertility Preservation Center
- Laparoscopy
- Hysteroscopy
iDream CenterFields of Service
-
Polycystic Ovary Syndrome/
Ovulation Disorder - Ovarian Dysfunction
- Male Infertility/Sperm Bank
- Artificial Insemination
- In-Vitro Fertilization
- Selection of Best Embryo
- Creating the Optimum Condition for Implantation
- Recurrent Miscarriage/Recurrent Implantation Failure
- Preimplantation Genetic Diagnosis
- Fertility Preservation Center
- Laparoscopy
- Hysteroscopy
-
Polycystic Ovary Syndrome/Ovulation Disorder
- Polycystic Ovary Syndrome
- Polycystic Ovary Syndrome is a set of symptoms characterized by irregular menstrual periods causing an increase in male hormones (leading to excess body and facial hair, acne, etc.) or the polycystic shape of the ovary on ultrasound. The symptoms are commonly witnessed in about 10-15% of the women of childbearing ages, and frequently occur from the early age of youths. They may temporarily disappear after the emergency at the early stage to occur again later. The symptoms range from simple irregular menstrual periods to all complications associated with the syndrome. Instead of full recovery, this syndrome should rather be continuously managed.

Causes and Mechanism
No exact causes are known for this syndrome. Complex actions including genetic factors or insulin resistance may be causes, and the disorder in the secretion of hormone that is induced by this syndrome cause diverse clinical patterns and complications. Insulin resistance is most commonly caused by obesity, and it can also be witnessed in thin women.
Symptoms
table title Irregular Menstrual Period Oligomenorrhea (less than eight menstrual periods in a year), amenorrhea, very small quantities of menstruation, large irregular bleeding, etc. Skin/Appearance-related Symptoms Acne, excess body and facial hair, hair loss, darkening skin Inferility Overweight, obesity Male type obesity (abdominal obesity) can occur, but not always so. Complications of the Syndrome
- Obesity
- Diabetes (noninsulin dependent)
- Cardiovascular disorders
- Solenoma, Endometrial Hyperplasia
Tests Required for Diagnosis
No single-test is currently available for diagnosing the syndrome.
Blood Test
As the syndrome cause diverse disorders in hormone secretions and show the symptoms that can also be witnessed with other diseases, a thorough test is important, which requires the testing on the morning of the 2nd-3rd day of menstruation.
- Female and male hormones : FSH, LH, Testosterone
- Tests of thyroid, lactogenic hormone and adrenal disorders : TSH, PRL, DHEAS, 17-OH-progesterone For the prevention of diabetes and cardiovascular disorders, tests of fasting blood sugar and insulin levels, glucose tolerance, lipids, etc. may also be required.
Ultrasound Test
A patient is diagnosed with the syndrome when she is found to have at least five cysts sized under 10mm in the ovary. Such small cysts are the ones remaining from the follicles that failed to grow further for ovulation. As the number of cysts increases, the ovary becomes larger, showing distinct disorders in hormone secretions.
Obesity Test
Height, Weight and BMI
Treatment of the Syndrome
No single treatment method is currently available to completely cure the syndrome, but there may be diverse methods for controlling it. Such treatments can help improve the symptoms but if the treatments are suspended, the symptoms and the disorders in hormone secretions can recur, requiring continued treatment efforts to reduce the risk of the occurrence of complications.
table title Weight Reduction The primary method recommended for the overweight or obese women. A 5-7% reduction of weight can contribute to normal ovulation and long-term prevention of complications. Therefore, overweight or obese women need to begin the treatment of the syndrome with weight reduction.
However, weight reduction requires a very high level of self-control, leading to repetitive failures. MizMedi Hospital's specialists in endocrinology and family medicine provide diverse services in the hospital's Obesity Clinic.Ovulation Inducing Agent;
Oral or InjectionInduced ovulation for a higher possibility of pregnancy Contraceptives Besides the contraceptive effects, drugs can reduce male hormones to improve excess hair, acne, and etc. Progesterone Agent Endometrium can be protected by inducing regular menstruations. Insulin Lowering Drugs; Metformin, etc. Lowering the levels of insulin and male hormone can improve the symptoms, induce regular ovulations and prevent complications. The possibility of pregnancy can also be raised by taking other ovulation including drugs at the same time. This can lower the rates of spontaneous abortion and gestational diabetes, which can be seen in the syndrome. Ovary Drilling This is a surgical technique of puncturing the membranes surrounding the ovary with an electric surgical needle using laparoscopic procedures, which is employed when the patient does not show response to the ovulation inducing agent. Unlike an abdominal operation, it seldom causes adhesion around the ovary, and 40% of the patients begin regular ovulations after procedure. However, surgical procedures are employed only when medications have been failed. Other Treatments Based on Symptoms For the treatment of the excess body and facial hair, acne, and etc., antiandrogenic agent, shaving, decolorizing, electrolysis, laser treatment, and etc. can be used. Insulin Resistance and Polycystic Ovarian Syndrome
Currently, the exact cause of polycystic ovarian syndrome is not known but the syndrome is thought to be caused by complex actions of diverse causes as well as genetic factors. In recent years, insulin resistance is drawing an increased attention as one of the causes and, diabetes is actually being frequently found in the diagnostic process of the syndrome.
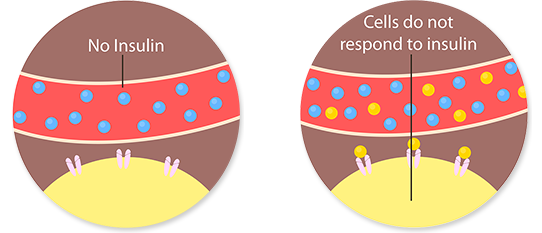
What is Insulin Resistance?
Insulin resistance is a condition in which insulin is not effectively used for controlling the level of sugar though it is normally secreted. Insulin resistance causes the human body to need more insulin for the normal control of sugar, resulting in higher levels of insulin in blood. This again causes to increase male hormones, which cause the characteristic symptoms like acne, anovulation and infertility.
The most common cause of insulin resistance is obesity, but it is also found in thin women as well. Insulin resistance causes metabolic syndrome which is characterized by diabetes and hyperlipidemia, and is an important risk factor for cardiovascular disorders and diabetes.Treatment of Insulin Resistance - Metformin
As the relations between polycystic ovary syndrome and insulin resistance were revealed, insulin lowering drugs began to be used in the treatment of the syndrome, leading to a more fundamental treatment of the syndrome. The most commonly used drug is metformin, which is a blood sugar depressant for oral medication. Metformin enhances the reaction of insulin to lower the levels of blood sugar and insulin. This leads to lower levels of male hormones to improve diverse symptoms of polycystic ovary syndrome and prevent long-term complications. Additionally, a single treatment can induce normal ovulations and co-medication with other ovulation inducing agents can contribute to a higher possibility of pregnancy. Unlike ovulation inducing agents, however, it does not provide the risk of multiple births, and unlike other blood sugar lowering drugs, it actually provides no side effect of hypoglycaemia.
The most common side effects of metformin are the ones related to the digestive system including nausea, vomiting stomachache and diarrhea, and these symptoms can be mostly improved within several weeks from the start of treatments. As the improvement is proportional to the amount of drugs, the quantities can be gradually increased. In the patients of the disorders of the kidney, liver and lungs, there is an increased risk of complications, requiring consultation with the doctor prior to medication for the test including a blood test.Conclusions
The most important thing in the control of polycystic ovary syndrome is the appropriate recognition and information about the syndrome. In this sense, attention should be continuously paid to the syndrome before and after childbirth, and continued consultations with the specialists in the field are also recommended.
-
Ovarian Dysfunction
Ovarian Dysfunction
The function of the ovary is directly related with a woman's age. The number of eggs the ovary contains at the time of her birth is already determined, and, as the number continues to decrease from the first menarche to menopause, the function of the ovary gradually decreases. The symptoms can be seen in the patients who have received anti-cancer treatment, radiotherapy, or the past General Surgery performed on the ovary, and the functions can also be affected by the past General Surgery that can reduce blood supply to the ovary, inflammation or, sometimes, smoking.

Predictive Test of the Ovarian Function
The tests for predicting the functions of the ovary include FSH test, estradiol value test, AMH test and ultrasound. The ultrasound test evaluates the ovarian function by counting the number of small follicles inside the ovary.
table title FSH and Estradiol Value Tests Higher levels than the standards of follicle-stimulating hormone (FSH) that is secreted from the pituitary gland, and estradiol that is secreted from the ovary mean the function of the ovary has been lowered. In other words, if the function of the ovary is lowered, more hormones need to be secreted from the pituitary gland to stimulate the ovary for ovulation. AMH Test Anti-Müllerian hormone (AMH) is the hormone secreted from the small follicles inside the ovary, and its lower level means a lower number of eggs. Though the number of eggs is not necessarily related to a higher possibly of pregnancy, a lower level can cause a reduced possibility of pregnancy, requiring more active attempts for pregnancy.
The patients who have ovarian dysfunction despite a young age are recommend to receive procedures that can raise the possibility of pregnancy. The functions of the ovary cannot be improved with only one occasion of treatment and, as the functions continue to worsen as the patients age, time is essential for pregnancy. In this sense, patients are sometimes advised to directly take IVF without artificial insemination.Symptoms
The lowered function of the ovary means a lower response to hyperovulation that is employed in in-vitro procedure. The results of the studies on the pregnancy rates of the patients with the lowered ovarian response differ, and one of the reasons is the fact that the ovarian dysfunction is not clearly defined yet. The related experts who participated in the expert meeting held in Bologna in 2010 agreed on the definitions of the ovarian dysfunction to the effect that a patient has the ovarian dysfunction if she satisfies at least two out of the following conditions:
table title Showing the Following Symptoms Having the following risk factors: Over 40 years of age, endometrioma of the ovary on ultrasound, past experience of ovarian General Surgery, past experience of anti-cancer treatments, genetic abnormalities (Turner syndrome, FMR1 premutation), pelvic inflammation, damaged fallopian tube, shortened menstruation cycle Having Showed a Lowered Response in the Past In-Vitro Procedure Less than three eggs were collected despite the daily injection of 150 IU FSH minimum, or the procedures were suspended due to the growth of less than three follicles. Results of the Ovarian Function Test Having Shown Dysfunction - Antral follicle count is under 6
- AMH is under 1.0ng/ml
- FSH is at least 12IU/ml on the third day of menstruation
Dealing with Ovarian Dysfunction
If the patient experienced lowered ovarian response in the past or did not show a positive response to the first IVF attempt, how should IVF be done? There is no single answer to this question.
The answer depends on the conditions of the patients including those who are predicted to show a normal response and need higher doses of injection for the response of hyperovulation.
In case the number of eggs do not exceed despite the IVF procedure, the only egg that is naturally ovulated is retrieved or an ovulation inducing agent is medicated while minimizing the use of injections.
As assistive alternatives, some dietary supplements and the injection of growth hormone are sometime used, and though these are not clinically tried, they still are helpful to some extent.
-
Male Infertility/Sperm Bank
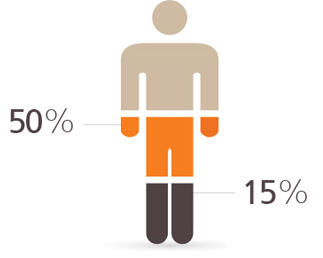
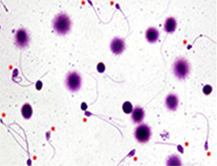
- Necessity of Examining Male Infertility
- In general, at least 15% of married couples are said to be suffering from infertility. Infertility is the inability to conceive a baby for at least one year despite normal sex life without contraception. In these couples, husbands are said to be responsible for about 50% of the causes of infertility. Therefore, in infertility cases, male infertility should be checked.
Causes of Male Infertility
table title Medical Causes Varicocele, infection, ejaculation problem, antisperm antibody, cryptorchidism, hormone problems, sperm duct blockage, tumor, chromosome abnormalities, past surgeries, and etc. Environmental Causes Chemical substances for industrial use, heavy metals, radiation, exposure of testicles to high temperature, etc. Lifestyle Causes Excessive use of drugs, heavy drinking, smoking, stress, overweight, etc. Examination of Male Infertility
table title Physical Exam Testicles and scrotum, seminal duct, varicocele, and etc. should be examined. Medical History Disease, past General Surgery, medication, genetic disease, intercourse, and etc. should be checked. Semen Analysis Maintain abstinence for 2-3 days. If normal, one occasion of semen analysis is sufficient, but if any abnormal sign is suspected, one or two more examinations may be recommended. In the examination of semen, it checks the quantity of sperm, sperm count, motility, leukocyte count, and etc. are checked. Semen DNA Exam If there is varicocele, or the assisted reproduction procedure continues to fail, semen DNA examination aimed at checking DNA damages is recommended. Hormone Test Hypothalamus, pituitary gland and testicles are important in the production of sperm and male hormones. FSH, LH, Estrogen, Testosterone, Prolactin, and etc. should be checked. Urine Test Performed after semen exam, this test is aimed at checking infections that can affect pregnancy. Retrograde ejaculation, by which semen is redirected to the urinary bladder, can also be checked with the urine test. Genetic Testing Genetic testing is conducted in the cases of low sperm count, aspermia or recurrent miscarriages. Other Blood Tests Overall conditions including infections that can affect pregnancy, liver functions, hyperlipidemia are checked. Ultrasound Test Varicocele, abnormalities of testicles or epididymis, etc. are checked with testis ultrasound, and prostate, ejaculatory duct, seminal vesicle, etc. are checked with prostate ultrasound. Treatment of Male Infertility
table title Surgical Treatment If diagnosed with varicocele, the enlarged blood vessel should be surgically removed. And in the case of obstructive azoospermia, vaso-epididymostomy should be performed to reconstruct the passageway of sperm. Those who received vasectomy in the past can receive vaso-epididymostomy. Infection Treatment Treatment of infections with antibiotics can also raise the possibility of pregnancy. Hormone Treatment This can be performed on the patient of infertility having hormone problems. Alternatrive Drugs Arginine, Carnitine, Coenzyme Q10, Folic acid, Glutathione, Omega fatty acids, Selenium, Vitamine A, Vitamine C, Vitamine E, Zinc Good Habits for Healthy Pregnancy
- Quit smoking
- Reduce or quit alcohol consumption
- Maintain normal weight
- Avoid exposure to the environment in which the temperature of testicles rise, including sauna.
- Avoid exposure to the diverse environmental hormones.
FAQ about Male Infertility
table title What is varicocele? Being one of the common causes of infertility visiting the hospital at the rates of 20-30%, varicocele is an abnormal enlargement of the pampiniform venous plexus in the scrotum. How Does it Cause Infertility? Testes are located outside the body to keep them at a lower temperature than the body. The major functions of testes are production of sperm and secretion of male hormone, and, if there is varicocele, the testes are put in a bad environment. It can cause raised temperature of testes, diminished supply of oxygen, reduced reproductive organ hormones, toxic substances to negatively affect the motility, shape, count, etc. of sperm, and can sometimes cause pain on the scrotum. How Is It Diagnosed? Depending on the level of symptoms, it can be divided into three levels, with the most enlarged one being visible with the naked eye. It can also be diagnosed with simple digital exploration, and also sometime using ultrasound. In terms of anatomy, it mostly occurs on the left side of the scrotum, but can sometimes occur on both sides. Should This Always Be Treated? General Surgery for varicocele is, in general, performed for pregnancy. Cases in which neither pregnancy is wanted nor pain is caused and no change in the sizes of testes are not considered as surgical implications.. How Is It Treated? While there are diverse methods of treatment, the surgical removal using the microscope is known to show the highest success rate and lowest complications. The patient can be discharged on the next day of the General Surgery. What Are the Advantages of Surgical Treatment After General Surgery, the symptoms of varicocele improve in 60-80% of the patients, raising the possibility of natural pregnancy to about 40-50% within a year and to about 70% within two years. -
Artificial Insemination
- Definition of Artificial Insemination
- Artificial insemination (AI) is the deliberate method of receiving semen from a husband in a woman's ovulation period, treating it with a special culture fluid, and then collecting only sperm with good motility and injecting it directly into a female's uterus through a thin tube.
Major Considerations For AI
What serves the most important role in natural conception is sperm having a good motility and a sufficient amount of cervical mucus. Therefore, the followings should first be considered:
In case sperm's motility is diminished or cervical mucus is not properly secreted due to cervical conization, and etc., AI is preferable than natural conception for a higher possibility of pregnancy.
AI may also be considered if natural conception does not occur for at least six months to one year despite no particular abnormalities found in the infertility exam.
AI and In-Vitro Fertilization (IVF)
As AI should be implemented inside the body, at least one fallopian tube should be properly functioning, and, IVF is strongly recommended when both tubes are blocked or any significant ovarian dysfunction or significantly lowered conditions of the sperm.
※ While AI may be conducted based on the natural menstrual cycle, hyperovulation is mostly used for a higher possibility of pregnancy. The rate of successful pregnancy per cycle is about 20%.
-
In-Vitro Fertilization
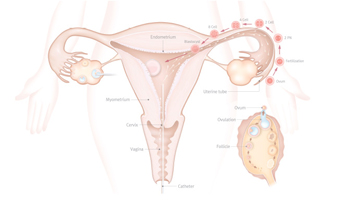
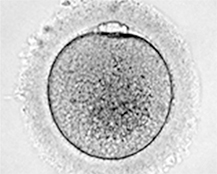
- Definition of In-vitro Fertilization
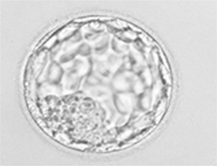
- In-vitro fertilization, or "in-vitro fertilization-embryo transfer" (IVF-ET) in full, is a process of fertilization in which an egg is taken out from a woman and, after its fertilization with sperm outside the body and embryo culture for 2-5 days, is transferred to the endometrium.
Procedure

- Stage 1: Ovarian Hyperstimulation
- In the natural menstrual cycle, one egg is ovulated a month. Ovarian hyperstimulation is the stimulation to induce development of multiple follicles of the ovaries for higher possibilities of pregnancy. The method of inducing ovulation is determined in consideration of diverse factors including the age and ovarian function of the patient, and the results of the past inducement.
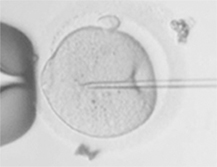
table title A. Long Protocol From one month before beginning IVF, GnRH agonist is medicated. Hypodermic injections are provided 7-10 days before menstruation, and as menstruation begins, ultrasound and hormone exams are performed to check if the conditions are appropriate for inducing ovulation, and gonadotrophin is injected to induce hyperovulation. The state of ovulation is checked through ultrasound and blood tests every 2-3 days on average. The stage, though it is long due to injections, is characterized by its stability. B. Short Protocol From the third day from of menstruation, gonadotrophin is injected, and when follicle is grown to a certain size, GnRH antagonist is injected to prevent premature ovulation and retrieve egg. When compared to a long protocol, the growth of follicle may not sometimes be even, but the period for injections is relatively short, with the rates of pregnancy are similar. C. Mild IVF Mild IVF is used to prevent the side effects associated with high stimulation IVF and uses a lesser amount of injections for inducing ovarian hyperstimulation. In general, an ovulation inducing agent is also used to use a lesser amount of injections. D. Natural Cycle IVF In this method, no hyperstimulation-inducing injection is used to retrieve the egg on the day of natural menstruation. The process is simple and costs less, but exclusively used in the group that shows an extremely low egg retrieval rate. - Stage 2: Egg Retrieval and Sperm Prepration
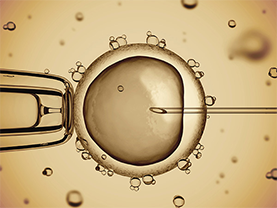
table title A. Egg Retrieval As the mature follicle is monitored on ultrasound, gonadotrophin is injected and the egg is retrieved after about 34-36 hours later. In most cases, the eggs are retrieved from the patient using a transvaginal technique called transvaginal oocyte retrieval, involving an ultrasound-guided needle piercing the vaginal wall to reach the ovaries. B. Sperm Preparation Sperm is prepared for fertilization on the day of egg retrieval, and abstinence 2-3 ahead of sperm preparation is recommended. Sperm is collected in the container through masturbation, and, depending on the situation, can be collected from the frozen sperm or through a surgical procedure. - Stage 3: In-Vitro Fertilization and Culture
- Upon retrieval of the egg and sperm, they are put on a culture dish containing culture medium for fertilization. In general, it is left for natural fertilization, otherwise intracytoplasmic sperm injection (ICSI) is also opted. The fertilized embryo is cultured for about 3-5 days.
- Stage 4: Embryo Transfer
- The fertilized embryo is inserted to the endometrium using a catheter. The locations of the catheter and embryo are checked under abdominal ultrasound. Depending on the age of the patient, conditions of the embryo and number of days of culture, 1-3 embryos are transferred. No anesthesia is required, and the patient can return to normal daily life after taking a rest for about 10 minutes.
- Stage 5: Luteal Support
- Luteal support begins after egg retrieval. In most cases, progesterone agent or gonadotrophin agent is used, which can be injected, inserted through the vagina or orally administered. Luteal support contributes to the implantation of the embryo and embryogenesis.
-
Selection of Best Embryo
- Incubation of The Best Embryo For Transfer and Establishment of Selction System
- iDream Clinic has introduced the incubation room having clean room facilities and the air shower system to completely block fine dust and provide the optimum atmospheric environment for in-vitro cultivation of the embryos.
The clinic also has G210 InviCell Long Term Incubator with individual chambers that help secure the individual incubation spaces for each embryo to achieve higher rates of pregnancy, and Primo Vision Time Lapse embryo monitoring system that allows for monitoring the growth stages of the embryo in the optimum conditions, contributing to the higher rates of pregnancy based on the best embryos selected. 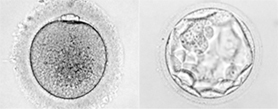
Embryo Incubator with Individual Chambers
Establishment of Latest Embryo Culture System

Latest Embyo Incubator That Is Recently Introduced
- Controls electromagnetism that occurs in the traditional incubators
- Uses advanced temperature system to maintain the culture temperature cycle similar to human body
- Individual cuture spaces for embryos are provided per patient to provide an environment that does not affect other embryos
And, considering the fact that the long term embryo culture method is being widely adopted in recent years, the culture method using ambient humidity helps prevent microbiosis of the embryos, and the individual embryo culture spaces contribute to preventing cross-infection.
Embryo Incubation Using the Latest Embryo Incubation System
- Maintaining embryos in the best conditions
- Such conditions contribute to higher rates of pregnancy
Time-Lapse Embryo Monitoring System
Last time-Lapse Image of the Embryos
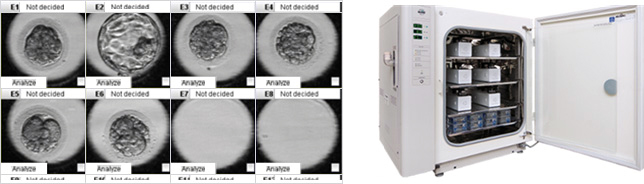
Last time-Lapse Image
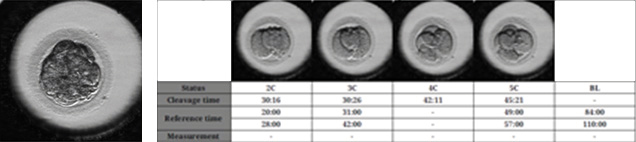
In checking the developmental stages of embryos using the conventional microscope, there have been limits to checking the division and morphological development of abnormal embryonic cells. As this time-lapse monitoring system is capable of checking the growth stages of embryos on a real-time basis, the best embryos for transfer can be selected, which contributes to higher rates of pregnancy.
Additionally, instead of having to regularly take out the embryos from the incubator to monitor the conditions in the past, the system allows for monitoring the developmental stage of embryos on a real-time basis using the monitor connected to the microscope that is inside the incubator, which contributes to block harmful substances entering from outside and reducing the stress caused by the changes in the environment. -
Creating the Optimum Condition for Implantation
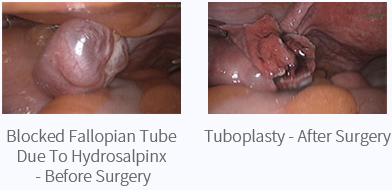
- Hydrosalpinx
- A hydrosalpinx is a distended and blocked fallopian tube filled with serous or clear fluid, which interferes with natural conception. The substances secreted from the fluid also affect the conditions of the embryo and the uterus, causing infertility.
Some studies showed that removing the fallopian tube having hydrosalpinx contributes to a higher success rate of pregnancy, but diverse studies are being also conducted in relation to whether the fallopian tube should be removed regardless of the conditions of the tube. 
- Endometrial Stimulation
- In IVF, one of the causes of repetitive failures of pregnancy despite transfer of a healthy embryo is the conditions of the endometrium. In recent years, studies are actively conducted regarding this issue, and one of the alternatives is to make a cut artificially on the endometrium to stimulate diverse active factors that promote growth of the endometrium.
More studies have yet to come to decide that the endometrial stimulation actually raises pregnancy rates, but the results so far reported show that a number of cases in which the pregnancy rates have been raised in the groups of people who failed in pregnancy despite repeated IVF procedures. However, as this is a procedure that can be easily performed, many studies are now in progress. 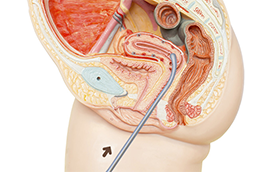
- Gonadotropin-releasing Hormone Agonist
- The consequences of providing gonadotropic hormone during the implantation phase are not clearly known. There are at least such hypotheses that gonadotropic hormone acts upon pituitary gland to promote the secretion of corpus luteum hormone, and this corpus luteum hormone acts upon endometrium, and directly acts upon the gonadotropic hormone receptor existing in endometrium to affect endometrium. Many studies in this area are now in progress.
However, a number of studies have asserted that providing gonadotropic hormone helps raise the success rate of IVF. 
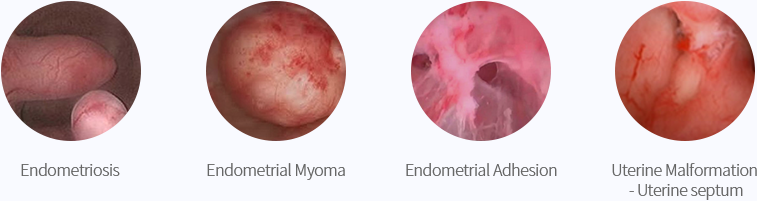
- Hysteroscopy
- Hysteroscopy is the most useful method of inspecting pathology in the uterine cavity by endoscopy with access through the cervix. This can be used to remove polys or adhesions which may not be readily detected with ultrasound in the case of repetitive implantation failures.
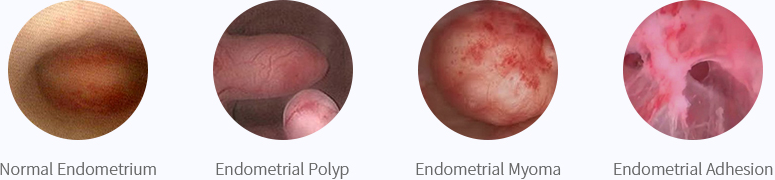
- Normal Endometrium
- Endometrial Polyp
- Endometrial Myoma
- Endometrial Adhesion
-
Recurrent Miscarriage/Recurrent Implantation Failure
- Definition of Recurrent Miscarriage
- Recurrent miscarriage is defined as three or more consecutive pregnancy losses before 20 weeks of gestation. But in accordance with the recent studies showing that the risk of miscarriage in those who experienced two consecutive miscarriages is not different from the risk in those with three consecutive pregnancy losses, the examinations on recurrent miscarriage are currently conducted on the women who experienced two consecutive miscarriages.

Causes of Recurrent Miscarriage
table title Genetic Factors
(3-6%)These are miscarriages caused by chromosomal disorders involving parental karyotype, and can be determined by examining the chromosomes of both partners. Anatomical Factors
(12-16%)Anatomical defects of the uterus including bicornate uterus and septate can cause recurrent miscarriages or infertility. Endocrine Factors
(17-20%)These factors refer to hormonal and metabolic imbalances. Imbalances in diverse hormones affecting pregnancy and the retention of pregnancy are such factors, which include such metabolic imbalances as thyroid dysfunction, diabetes and polycystic ovarian syndrome. Reports say hypothyroidism or the autoimmune disease of the thyroid can cause an increased risk of miscarriage, and the imbalances in glycometabolism due to the polycystic ovarian syndrome and diabetes can also cause higher rates of miscarriage. Immune Factors and Thrombophilia
(20-50%)These factors refer to the autoimmune disease like the antiphospholipid antibody syndrome, increased activities of the natural killer cells, etc., and thrombophilia caused by these factors are known to raise the rates of miscarriage. Infection (0.5-5%) A certain vaginitis and pelvic inflammatory disease are associated with the early-stage miscarriages. Unexplained (10%) These cases are the ones whose causes are not determined after having performed all of the above-mentioned examinations, which account for a 10% of the entire cases. Diagnosis and Treatment
table title Genetic Factors Appropriate consultations on the genetic factors including the parental chromosomes are needed, and the preimplantation genetic diagnosis (PGD) can also be useful. Anatomical Factors - The disease can be accurately diagnosed through the imaging of the Fallopian tubes, hysteroscope, laparoscope, etc.
- Uterine anomaly can be surgically corrected and treated using the hysteroscope.
Endocrine Factors - Endocrine factors can be easily diagnosed through a blood test, and the disease can be prevented through treatments.
- In the case of an imbalance in glycometabolism, the rates of miscarriage can be lowered through a balanced diet, administration of insulin sensitizer or the appropriate treatment of diabetes.
- In the case of thyroid malfunctioning, the rate of miscarriage can be lowered by maintaining the level of thyroid hormone at the normal level through supplementing thyroid hormone.
Immune Factors and Thrombophilia - The disease can be treated through a blood test for checking the functions of diverse autoantibodies and immunocytes.
- Aspirin and heparin injections are known to be useful in treating thrombophilia, and immunosuppressants including immunoglobulin can also be useful.
Infection The disease can be diagnosed through the examination of vaginal secretion, and can be easily treated using antibiotics. -
Preimplantation Genetic Diagnosis
- Definition of Preimplantation Genetic Diagnosis
-
Definition of Preimplantation Genetic Diagnosis
Preimplantation genetic diagnosis or preimplantation genetic screening inspection is a clinical method of examining chromosome abnormalities or genetic diseases using the cytogenetic or molecular genetic method upon the fertilized eggs during the procedure of the assisted reproductive technique.
Preimplantation genetic diagnosis is employed in the patients with a family history having a risk of giving birth to a baby with chromosome abnormalities (mutual translocation or Robertsonian translocation) or severe monogenetic disorders, and a consultation with the specialist is required to determine whether the diagnosis can be employed or not.
Preimplantation genetic screening inspection is mostly employed in the senior patients or those who experienced recurrent miscarriages, and the inspection of numerical aberrations of chromosomes is typically performed. All of these methods are performed before implantation, and only the normally fertilized egg is implanted in the uterus to help give birth to a healthy baby. 
Procedure of Preimplatation Genetic Diagnosis
-
01 Separation of Embryonic Cells
-
02 Examination of Genetic Disorders/Chromosomes
-
03 Implantation of Normal Embryo/Gestation of a Healthy Fetus/Baby
Separation of Embryonic Cells
Cells are collected from the day-3 embryo (8-cell embryo) or the day-5 embryo (blastocyst) using the embryo micromanipulation technique. Collecting the cells from each embryo does not affect the generation and implantation of the embryo and gestation at all, and the collected blastocytes are used for a molecular cytogenetic examination before implantation.

Examination of Genetic Disorders and Chromosomes
This is the simplest method to diagnose the numerical aberrations of chromosomes in the embryo.
For the process, the FISH (fluorescence in situ hybridization) method by which the fluorescent probe is used is employed to conduct genetic examination. This genetic examination is mostly employed for, among the patients of subfertility, the relatively aged women and those who experience recurrent miscarriage or tend to lose pregnancy during in vitro fertilization. The numerical aberrations of chromosomes are checked mostly upon the X and Y sex chromosomes related to Turner's syndrome and Klinefelter's syndrome, chromosome 21 related to Down syndrome, chromosome 18 related to Edwards syndrome, chromosome 13 related to Patau syndrome, and etc.
The whole DNA is amplified from the embryonic cells that are collected using the recently developed WGA (whole genome amplification) technique, and the chromosomes are checked for aberration using the array CGH technique.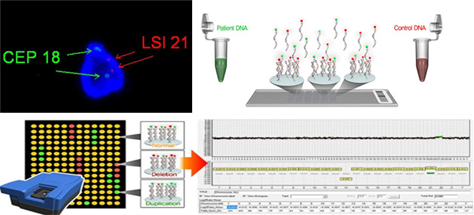
Advantages of the Above Methods
- More prompt and accurate analyses of the entire chromosomes compared to FISH
- Accurate diagnosis even in the single cells through the DNA amplification technique
- Contributing to checking the normal chromosomes of the embryo in case one of the parents has balanced translocation
- The increased rates of pregnancy by implanting the normal embryos only that are checked through the genetic examination
-
Fertility Preservation Center
- Fertility Preservation
-
All women are born with approximately one million reproductive cells. Of the cells, about 400-500 cells are ovulated from the first period to menopause, and the rest of the reproductive cells are gradually decreased in the number through apoptosis. As women age, the number of cells continues to decrease and menopause comes when these reproductive cells are depleted.
The number of reproductive cells begins to decrease at a faster pace after the age of 35, and the quality of ova also is also lowered. The index that reflects the number of the remaining reproductive cells is called the ovarian reserve, which can be evaluated through a blood test or ultrasound examination and is used as the index for childbearing capability.
As the ovarian reserve is already decreased several years before menopause, the fact that a woman has periods now does not necessarily mean that she can get pregnant. Therefore, healthy reproductive cells need to be protected before the ovarian reserve is reduced. In particular, a cancer patient who is receiving chemoradiotherapy must protect her fertility in advance. Also, due to the recent trend of late marriage, unmarried women, even if they are currently healthy, need to protect their reproductive cells in advance as the functions of the ovary can weaken. 
Ovarian Reserve Exam
- Ultrasound Exam
- Hormone Exam (LH/FSH/E2)
- Antimullerian Hormone (AMH) Exam
Those Who Need Fertility
- With past experience of ovarian General Surgery
- Having endometriosis
- Having family history of premature menopause
- Having to undergo radiotherapy due to a detected cancer
- Women suspected of diminished ovarian function
- All women who wish to preserve ovarian reserve
How to Preserve Fertility
Embryo Freezing After IVF
Embryo freezing (embryo cryopreservation) after IVF is adopted in the women who cannot conceive at the moment due to cancer treatment, etc. and whose level of fertility is significantly lowered. This method of freezing the embryos that are fertilized with the spouse's sperm has been showing high success rates (about 50-60% of pregnancy after transfer of the frozen embryo) of pregnancy with extensive clinical experiences. However, this method cannot be adopted for unmarried women as their eggs cannot be fertilized.
Ovarian Tissue Freezing
Ovarian tissue freezing is mostly employed in young cancer patients for whom hormone hyperstimulation cannot be opted. In such patients, their ovarian tissues are surgically collected using laparoscopy, etc. before conducting cancer treatment that can cause diminished ovarian function and, upon completion of cancer treatment, the frozen tissues are transplanted upon subcutaneous tissues or inside the abdominal cavity. In the laboratory, the ovary’s outer layer (called ovarian cortex) is cut into small strips and frozen. Despite some advantages including no need for the period of hormone hyperstimulation and the recovery of fertility after transplant and endocrinal functions, its rate of successful pregnancy is still low.
Freezing Eggs After Egg Collection
In this method, a multiple number of eggs are collected in one menstrual cycle of the unmarried women through the minimum level of hormone stimulation and freeze them for preservation. This method is conducted in a similar manner to IVF, but the mature eggs are immediately frozen without fertilization for future use. This method is relatively simple and does not require surgical procedures, but the time for hormone hyperstimulation is required for those patients who have to undergo cancer treatment.
-
Laparoscopy
- Laparoscopy and Infertility
- Laparoscopy is a useful means for checking the exact conditions of the fallopian tube. While it can also be used for checking pelvic adhesion or endometriosis, it needs anesthesia and is an invasive exam method. Therefore, it is not used as the primary exam means and is opted on when the patient has a disease that should be treated like hydrosalpinx

Treatment of Infertility
If the Fallopian Tube has Abnormalities
The fallopian tube is an important area where the union between the egg and sperm occurs. Abnormalities found here may require surgical treatment depending on the conditions, and if it is judged normal function of the tube may not be possible after General Surgery, IVF needs to be considered.
Cervical Adhesion and Hydrosalpinx
If the fallopian tube is adhered to the neighboring areas and only its tip is blocked, the tube should be opened. Hydrosalpinx acts to reduce the rate of pregnancy by half and can cause miscarriage, and therefore, when conducting IVF, tubal ligation or tubectomy is generally implemented for a higher rate of pregnancy.
Tuboplasty
If the fallopian tube is severely damaged or its ultrastructure is maintained, the function of the tube can be recovered by opening the blocked tip of the tube through tuboplasty. However, as tuboplasty can sometimes cause tubal pregnancy, IVF is more often conducted after tuboplasty if IVF has failed for multiple times.
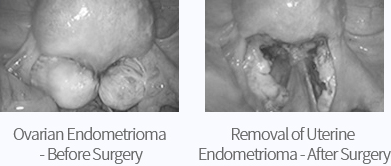
Treatment of Endometriosis of Infertiflity Patient
In the treatment of uterine fibroid that occurred in the ovary of a patient of infertility, maintaining the functions of the ovary is most important, and, in principle, it should not be removed if its size is about 4cm in diameter. General Surgery may be considered if there is a risk of hysterorrhexis due to the location of endometriosis or the pain is significant, but the functions of the ovary can be lowered after General Surgery.
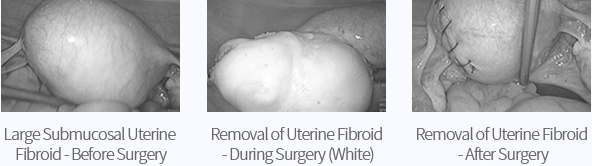
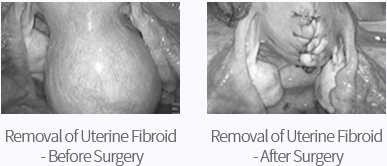
Treatment of Uterine Fibroid of Infertiflity Patient
Surgical treatment of uterine fibroid should be determined based on the size and location. In some cases, large submucosal uterine fibroid that changes the space inside the uterus or intramuscular fibroid is better to be removed using laparoscopy. Melting fibroids should be carefully selected as it can extend the uterus during pregnancy, causing rupture of the uterus.
-
Hysteroscopy
- About Hysteroscopy
- Hysteroscopy is the inspection of the uterine cavity by passing a long and thin hysteroscope through the vagina and cervix. Prior to insertion of the hysteroscope, fluids are introduced to expand cavity to facilitate the diagnosis of intrauterine pathology which may not be clearly seen with the ultrasound waves the video monitor and a surgical intervention is performed using fine surgical instruments.

Indications of Hysteroscopy?
- Check and treat uterus bleeding
- Remove tumors from the endometrium
- Remove the uterine septum
- Check the causes of infertility
- Remove the submucous uterine fibroid
- Separate the uterine adhesions
Upon checking the above lesions, the surgical instrument is inserted through another path attached to the hysteroscope to precisely remove or burn the lesions only.
Diagnosis of Endometrial Tumor and Hysteroscopic General Surgery (Clinical Case)
- Diagnosis: Inject physiological saline to examine the endometrial tumors using ultrasound examination
Uterus, uterine cavity (central black area), tumors inside the uterus - Tumors inside the uterus checked on ultrasound waves after hysteroscopy
- Procedure of hysteroscopic General Surgery
Surgical Procedures Per Type of Hysteroscope
Diagnostic hyteroscopy is performed using a fine hysteroscope without anesthesia, and usually takes about two to five minutes. Surgical hysteroscopy is performed under either general or local anesthesia, and, as it is finished within a short period of time, it does not require hospitalization and the patient can be discharged within 15-30 minutes after the General Surgery, allowing the patient to lead normal daily life from the next day. It is a relatively simple General Surgery involving no postoperative pain, while rarely the patient can suffer mild pain or stomachache, which can last from 30 minutes to eight hours. In most cases, the patient can get pregnant soon after the General Surgery.
Indications of Hysteroscopy
The lesions inside the uterus cause infertility, and the uterine anomaly and adhesions inside the uterine can cause recurrent miscarriages.
Hysteroscopic images of the uterine septum of the patient who experienced recurrent miscarriageComplications of Hysteroscopic General Surgery
Hysteroscopic General Surgery can cause postoperative infection, uterine perforations, vaginal bleeding, imbalance in electrolyte due to excessive supply of fluids, etc.

iDream ClinicHistory
-
History
-
2018
-
2018.7
- European Society of Human Reproduction and Embryology (ESHRE)
- The relationship between expansion degree of human blastocyst and clinical outcomes in ART In over 35 years old women, the clinical outcomes of Day 1~2 extended culture and transfer of thawed-Day 3 cleavage-stage embryos when compared with vitrified-thawed blastocysts.
-
2018.7
-
2017
-
2017.9
- The Korean Urological Association
- Defining Molecular Mechanisms Involved in the Ovarian Aging for Clinical Applications
-
2017.7
- European Society of Human Reproduction and Embryology (ESHRE)
- Molecular Networks underlying Ovarian Aging for Clinical Applications
-
2017.9
-
2016
-
2016.7
- International Society for Prenatal Diagnosis (ISPD)
- Case Report: Prenatal Diagnosed Rare Trisomy 16 Mosaicism
-
- European Society of Human Reproduction and Embryology (ESHRE)
- Defining Molecular Mechanisms Involved in the Ovarian Aging for Clinical Applications
-
2016.7
-
2015
-
2015.11
- Korean Society for Fertility Preservation (KSFP)
- Blastocyst Morphology Is Not Critical on Frozen-thawed Embryo Transfer for Improving Clinical Outcomes
-
2015.10
- American Society for Reproductive Medicine (ASRM)
- Is it necessary for intracytoplasmic sperm injection on patients with abnormal Sperm DNA fragmentation value in ART?
-
2015.11
-
2014
-
2014.12
- Asia Pacific Initiative on Reproduction (Aspire)
- THE RELATIONSHIP OF HALOSPERM TEST AND HYALURONAN BINDING ASSAY (HBA) IN SEMEN SAMPLE GROUPS CLASSIFIED WITH SPERM PARAMETERS SUCH AS COUNT, MOTILITY AND MORPHOLOGY.
-
2014.12
-
2012
-
2012.7
- Asia Pacific Initiative on Reproduction (Aspire)
- The effect of pregnancy outcome for intrauterine insemination (IUI) treatment medium supplemented with ethylenediaminetetraacetic acid (EDTA)
-
2012.7
-
2010
- 2010.12 J Womens Med. 2010 Dec;3(4):155-158. Published online Dec 10, 2010. http://dx.doi.org/10.5468/jwm.2010.3.4.155 Efficacy of luteal supplementation of vaginal sildenafil and oral estrogen on pregnancy rate following IVF-ET in women with a history of thin endometria: A pilot study
-
- American Society for Reproductive Medicine (ASRM)
- MICROSURGICAL ENUCLEATION OF TRIPRONUCLEAR OOCYTE TO RECONSTRUCT TWO PRONUCLEI IN an POOR RESPONDING 50-year old WOMAN BY MINIMAL OVARIAN STIMULATION.
-
2010.7
- European Society of Human Reproduction and Embryology (ESHRE)
- Effect of low-oxygen compared with high-oxygen atmosphere on the outcomes of in vitro fertilization, a prospective randomized study
-
2009
-
2009.7
- American Society for Reproductive Medicine (ASRM)
- A randomized controlled study for vitrification of cleavage-stage mouse embryos processed by two different methods: DMSO+EG or PROH+EG based method
-
2009.7
-
2008
-
2008.7
- European Society of Human Reproduction and Embryology (ESHRE)
- 1) Protective effect of antioxidant supplementation in sperm-preparation medium against oxidative stress in human spermatozoa.
-
- American Society for Reproductive Medicine (ASRM)
- (1) Human sperm DNA integrity assessed by single cell microgel electrophoresis (Comet assay) and its relationship to semen parameters and clinical outcome in IVF program
- (2) Early microsurgical removal of fragments can support the subsequent development of the fragmented human embryos by inhibiting the generation of new fragments
-
- Annual meeting of the Korean Society of ART
- (1) Causes and Prevention of multi-fetal pregnancy in ART
-
2008.7
-
2007
-
2007.11
- Korean Society for Assisted Reproduction’s autumn conference (received Excellent Paper Award)
- (1) The effect of microsurgical varicocelectomy on the DNA integrity of human sperm nucleus
-
2007.10
- American Society for Reproductive Medicine (ASRM)
- (1) What is a more effective protocol between conventional IVF and ICSI to fertilize oocytes with the sperm that shows strict morphology score 4-14%?
-
2007.9
- Korean Society for Assisted Reproduction’s autumn conference
- (1) Improvement of culture media for embryo
-
2007.7
- European Society of Human Reproduction and Embryology (ESHRE)
- (1) Protective effect of antioxidants supplemented into sperm preparation medium against oxidative stress in human spermatozoa
-
2007.2
- Korean Society for Assisted Reproduction’s spring conference
- (1) QC of ART Laboratory
-
2007.11
-
2018
-
History
-
1999
-
1999.10
American Society for Reproductive Medicine (ASRM)
- (1) Production of mature eggs through nuclear substitution and cytoplasmic
recombination of eggs in primordial follicle of mice - (2) Raised rates pregnancy using the biochemical assisted hatching in transplanting
cryopreserved embryo - (3) Stimulation of the expression of VIP and FISH receptors in fetal ovary
- (4) Clinical application of IVF using immature eggs collected without induced ovulatio
- (5) Expression of gonad-stimulating hormone and estrogen receptor genes in fetal ovary
- (1) Production of mature eggs through nuclear substitution and cytoplasmic
-
1999.7
Korean Society of Developmental Biologist
- (1) Roles of gonad-stimulating hormone receptor, estrogen receptor, aromatase and
cell adhesion molecule in affecting the forming of primordial follicle in the fetal
ovary - (2) Hypothesis on the growth inhibitory mechanism for primordial follicle in fetal
and infant ovaries
- (1) Roles of gonad-stimulating hormone receptor, estrogen receptor, aromatase and
-
1999.6
International Workshop on the early-stage forming of folliculus and egg
development- (1) Expression of gonadotrophin, estrogen, aromatase genes and cell cycle-related
proteins in human fetal ovary - (2) The effect of VIP on the synthesis of estrogen in human fetal ovary
- (1) Expression of gonadotrophin, estrogen, aromatase genes and cell cycle-related
-
1999.5
11th World Congress of In Vitro Fertilization and Human Reproduction Genetics
(World Congress of In Vitro Fertilization and Human Reproduction Genetics)- (1) Heightened rates of pregnancy in IVF using biochemical assisted hatching
- (2) Application of biochemical assisted hatching in assisted reproduction
-
1999.4
Japanese Society of Obstetrics and Gynecology
- (1) Raising the rates of pregnancy using assisted hatching in human assisted
reproduction - (2) Report on the rates of pregnancy raised by directly injecting sperm into the egg
cytoplasm using the sperm collected from cryopreserved testis tissues - (3) Report on successful gestation in infertility treatment using immature eggs
collected without inducing ovulation - (4) Report on successful gestation through preimplantation genetic diagnostics using
FISH in chromosomal translocation carrier showing recurrent miscarriages
- (1) Raising the rates of pregnancy using assisted hatching in human assisted
-
1999.3
7th symposium on the latest opinions on reproductive medicine
- (1) Diagnosis and treatment of aspermia
- (2) Medicine on somatic cells and embryo reproduction
-
1999.2
Korean Society of Developmental Biologist
- (1) Cytoplasm factor-induced genetic expression in the mouse’s early-stage embryo
and control of morphogenesis
- (1) Cytoplasm factor-induced genetic expression in the mouse’s early-stage embryo
-
1999.10
-
1998
-
1998.10
American Society for Reproductive Medicine’s invitational lecture:
"Assisted Hatching of Human Embryos"- (1) Expression of melatonin receptor genes in mouse gonad
- (2) Comparative analyses of the rates of fertilization, embryogenesis and rates of
pregnancy after intracytoplasmic sperm injection using the sperm collected from
the testis tissues thawed after cryopreservation - (3) Assisted reproduction using immature eggs collected without super ovulation
- (4) Study on the structural changes and hormonogenesis after explantation of the
18-week-old human ovary tissues thawed after cryopreservation - (5) Study on the in-vitro growth of the immature eggs of primordial follicle thawed
after cryopreservation
-
1998.8
Society for the study of Reproduction’s 32nd conference
- (1) Control of the genome activation by protein synthesis and phosphorylation
inhibition in mouse embryo
- (1) Control of the genome activation by protein synthesis and phosphorylation
-
1998.4
Korean Association of Biological Sciences’ spring conference
- (1) Control of morphogenesis due to the intracytoplasmic factors in the early embryo
of mouse - (2) Control of morphogenesis due to the substances originating from the eggs of
preimplantation mouse embryo
- (1) Control of morphogenesis due to the intracytoplasmic factors in the early embryo
-
1998.10
-
1997
-
1997.11
Korean Society for Reproductive Medicine’s autumn conference
- (1) Development of new IVF method without using super ovulation in IVF
-
1997.10
Society for the study of Reproduction’s 30th conference
- (1) Study on the control of the expression of integrin α1, α5, β3 genes by LIF in the IVF
process of mouse embryo
American Society for Reproductive Medicine
- (1) Sperm detection in the patients of oligoasthenozoospermia and intracytoplasmic
sperm injection using it - (2) Application of ICSI and ROSI in nonobstrusive azoospermia patient
- (3) Application of biochemical assisted reproduction using protein enzyme in human
ART program - (4) Study on the microdeletion of Y chromosome in Korean male infertility patients
and the frequency per area
- (1) Study on the control of the expression of integrin α1, α5, β3 genes by LIF in the IVF
-
1997.8
10th World Congress on In Vitro Fertilization and Assisted Reproduction
(World Congress on In Vitro Fertilization and Assisted Reproduction)- (1) Study on the detection of round spermatid in testis tissue specimen and the
application of human ART program
- (1) Study on the detection of round spermatid in testis tissue specimen and the
-
1997.5
5th International Congress of Andrology
- (1) Study on the microdeletion of Y chromosome in Korean male infertility patients
- (2) Analysis of the spermatogenesis process using the expression of DAZ and
Protamine -2 genes in testis tissue specimen
-
1997.4
Korean Association of Biological Sciences
- (1) Study on the microstructural change patterns of translucency during the hatching
of mouse embryo
- (1) Study on the microstructural change patterns of translucency during the hatching
-
1997.11
-
1996
-
1996.11
American Society for Reproductive Medicine
- (1) Report on successful normal gestation and childbirth after preimplantation genetic
diagnostics using FISH in the patients of chromosomal translocation-caused
habitual miscarriages - (2) Development of new assisted reproduction methods using biotic enzyme
- (3) Study on the enhancement of embryogenesis and the rates of pregnancy using
sperm acrosome reaction in the injection of sperm into the egg
Sisterhood with the Department of Obstetrics & Gynecology of the University of
Southern California (USC)Korean Society for Reproductive Medicine’s autumn conference
- (1) Analysis of Microdeletions in chromosome from Korean male infertility patients
- (1) Report on successful normal gestation and childbirth after preimplantation genetic
-
1996.10
Korean Society of Obstetrics and Gynecology’s autumn conference
- (1) Analysis of Y chromosome nonobstrusive azoospermia genes in Korean male
infertility patients
- (1) Analysis of Y chromosome nonobstrusive azoospermia genes in Korean male
-
1996.7
European Society of Human Reproduction and Embryology (ESHRE)
- (1) Study on the hatching and outgrowth of cryopreserved blastocyst mouse embryo
using diverse processing methods
- (1) Study on the hatching and outgrowth of cryopreserved blastocyst mouse embryo
-
1996.4
Korean Society of Obstetrics and Gynecology’s spring conference
- (1) Success of pregnancy using intracytoplasmic round spermatid injection (nation’s
first):ROSI
- (1) Success of pregnancy using intracytoplasmic round spermatid injection (nation’s
-
1996.11
-
1995
-
1995.6
Successful normal gestation after preimplantation genetic diagnostics using
FISH method in the patient of chromosomal translocation-induced recurrent
miscarriage(world’s first)Korean Society for Reproductive Medicine
- (1) Study on the application of intracytoplasmic sperm injection per cause of infertility
-
1995.5
Korean Society of Obstetrics and Gynecology’s spring conference
- (1) Study on the preimplantation genetic diagnostics using FISH method in
accordance with the number of the pronucleus during fertilization
- (1) Study on the preimplantation genetic diagnostics using FISH method in
-
1995.4
International IVF Society Award (IVF-ET) (received Excellent Paper Award)
- (1) Correlation between acrosome reaction and post-fertilization pronuclear formation
time during direct sperm injection into egg
- (1) Correlation between acrosome reaction and post-fertilization pronuclear formation
-
1995.3
Successful pregnancy using an innovative genetic diagnostics capable of detecting
diverse genetic diseases and gender by taking some part of the cells of the egg that
is 3-days into fertilization
-
1995.6
-
1994
-
1994.11
A clinical research paper from the nation on the significantly increased success
rates of in-vitro babies using proteolytic enzyme in
human body was presented in an academic conference (AFS) -
1994.10
Successful IVF using fresh testicular sperm and intracytoplasmic sperm injection
-
1994.4
Successful gestation using intracytoplasmic sperm injection
-
1994.11
-
1992
-
1992.10
Development of a simple surgical method of restoring the Fallopian tube
-
1992.4
Success of GIFT-ET combining the IVF and intrafallopian transplant
-
1992.10
-
1991
-
1991.10
Success of transplanting the fertilized egg using the uterus wall (world’s first)- transplant of the fertilized egg using a special needle
-
1991.10
-
1999

iDream ClinicAbout Clinic
-
iDream Clinic
MizMedi Hospital is the leader in the field of subfertility treatment and the nation’s first hospital to obtain the ISO accreditation in the field. The hospital provides the world-class management of eggs/sperm/embryos through the standardized service system and systematic management, and is equipped with the most advanced facilities and equipment to deliver effective and comprehensive care in assisted reproduction.
- Advanced IVF system, best environment for embryos
- The clinic is equipped with the culture room having clean room facilities and the air shower system to completely block fine dust and provide the optimum atmospheric environment for in-vitro cultivation of the embryos. The clinic also has Primo Vision Time Lapse embryo monitoring system that allows for monitoring the growth stages of the embryo in the optimum conditions. This system is capable of providing real-time monitoring and analysis from the outside of the externally fertilized embryo in the incubator until the day of transfer, preventing the inflow of external harmful substances and selecting the best embryo for transfer to contribute to higher rates of pregnancy. The clinic has also introduced the G210 InviCell Long Term Incubator with individual chambers that help secure the individual incubation spaces for each embryo to achieve higher rates of pregnancy.
- New embryo freezing method for increased rates of pregnancy
- For freezing the embryos remaining from the transfer process, vitrification is being increasingly adopted across the world. MizMedi Hospital uses our proprietary vitrification process, which, when thawed after freezing of such remaining embryos, shows over 60% rates of pregnancy.
- Enhanced effectiveness in male subfertility treatment through
inspection of sperm DNA fragmentation - The clinic inspects the level of DNA fragmentation of sperm (Halosperm test) to address the causes of the pregnancy failures and recurrent miscarriages caused by DNA damages and determine the optimum treatment and sperm processing for higher effectiveness in the treatment of male subfertility.
- Preimplantation Genetic Screening
- The simplest method of checking the numerical abnormalities of chromosomes in the embryo is the Fluorescence in situ hybridization (FISH) method, by which a fluorescent probe is used for specific chromosomes for genetic screening. This genetic screening is mostly employed for the age patients or those who suffer from recurrent miscarriages or have repetitively experienced pregnancy failures in IVF procedure. Inspection on the numerical abnormalities of chromosomes is mostly conducted on the X and Y sex chromosomes that are related to Turner syndrome and Klinefelter’s syndrome, trisomy 21 of Down syndrome, trisomy 19 of Edwards syndrome and trisomy 13 of Patau syndrome. By exclusively selecting the normal embryos, this process contributes to ever higher rates of pregnancy.
-
Research Staff of iDream Clinic
- Director
- Lee Hyeong Song
iDream Laboratory Team
-

- Infertility Research
- Kang Soo Man Senior
-

- Genetics Research
- Kim Sook Ryung Head
-

- Genetics Research
- Kim Young Joo Head
-

- Infertility Research
- Kim Joo Young Head
-

- Infertility Research
- Park Hae Keum
-

- Infertility Research
- Sim Mi ran
-

- Infertility Research
- Bo Mi Choi
-

- Infertility Research
- Kim Ji Eun
-

- Infertility Research
- Kim Ji Hyeon
-

- Infertility Research
- Song Seul gi
-
Research Fields of iDream Clinic
A. Spermatology and Andrology
(1) Sperm Induction of acrosome reaction in spermatozoa accelates development of fertilized human oocyte after intracytoplasmic sperm injection. (52th ASRM, 1996).Identification of round spermatid from testis biopsy and its application in human ART program. (10th World Congress on IVF & ART, 1997) Detailed semen analysis and ICSI in azoospermia-like infertile patients. (53th ASRM, 1997)
(2) AZF and Microdeletion Microdeletions of Y Chromosome in Korean Male Infertility Patients (5th ICA,1997) Evaluation of spermatogenesis by DAZ and protamine-2 gene in human testis biopsy (5th ICA, 1997) The Incidence of microdeletion and the frequency of AZFa, b, c deletion in male infertility patients. (53th ASRM, 1997)
(3) ART Application of ICSI or ROSI by testicular biopsy in non-obstructive azoospermia.(53th ASRM, 1997) Analysis of fertilization, embryonic development and pregnancy rates after ICSI using spermatozoa obtained from fresh or frozen-thawed testicular tissues (54th ASRM, 1998)
B. Oogenesis and Folliculogenesis
(1) Oocytes Production of mature oocyte from frozen-thawed primordial follicular oocyte by reconstruction with cytoplasm of full grown germinal vesicle(GV)-stage oocyte. (55th ASRM, 1999)
(2) Follicle In vitro Growth of Primordial Follicular Oocyte in the Frozen-Thawed Ovarian Tissue of Neonatal Mouse (54th ASRM, 1998) Steroidogenesis in the Frozen-Thawed 18 Weeks Human Fetal Ovarian Tissues Cultured In Vitro (54th ASRM, 1998) TGF βI and TGF βII were detected from fresh 18 weeks fetal ovarian tissue in human.
(3) Ovarian Endocrinology Expression of Melatonin receptor gene in mouse gonad. (54th ASRM, 1998) The synergistic effect of VIP and FSH in vitro on the expression of FSH receptor gene in human fetal ovary. (55th ASRM, 1999) Expression of receptor genes for gonadotrophins and estrogens, and biosynthesis of estrogen in mid-gestational stage of human ovarian tissues. (55th ASRM, 1999) Expression and localization of cell cycle-related proteins and receptor genes for gonadotropins, estrogen, and aromatase in human fetal ovaries; a preliminary study (International Workshop on Early Folliculogenesis and Oocyte Development,1999) The effect of vasoactive intestinal peptide on estradiol biosynthesis in human fetal ovarian tissue in vitro.(International Workshop on Early Folliculogenesis and Oocyte Development 1999)
C. Embryogrnrsis, Hatching and Implantation
(1) Embryology Regulation of embryonic genome activation and compaction by the transfer of cytoplasm transfer with inhibitors of protein synthesis or protein kinase in mouse. (32th SSR, 1999)
(2) Hatching Biochemical Assisted Hatching by Proteases Increased Pregnancy Rates in Human IVF-ET Program (1996' ASRM) Application of biochemically assisted hatching(BAH) by proteases in human assisted reproductive technology program. (53th ASRM, 1997) Improvement of pregnancy and implantation rate by biochemical assisted hatching in human IVF-ET. (11th World Congress on IVF & Hum Reprod Genet, 1999) Outcome of Biochemical Assisted Hatching in 1068 IVF-ET Cycles Using Pronase in Human Assisted Reproductive Technology. (11th World Congress on IVF & Hum Reprod Genet, 1999) Biochemical assisted hatching(BAH) increased the implantation and pregnancy rate in human cryopreserved embryo transfer. (55h ASRM, 1999)
(3) Implantation Regulation of integrin a1, av, and b3 gene expression by leukemia inhibitory factor(LIF) during blastocyst outgrowth in the mouse.(30th SSR, 1997)
D. ART
(1) Hatching and outgrowth according to various freezing procedures in mouse blastocyst cryopreservation. (12th ESHRE, 1996)
(2) Pregnancy from Translocation carrier patient with recurrent abortion by preimplantation genetic diagnosis using fluorescence in-situ hybridization. (52th ASRM, 1996)
(3) Assisted Reproductive Technology Program by Immature Oocyte Retrieval in Non-stimulated Cycle (54th ASRM, 1998)
(4) Clincial use of immature oocyte from normal and PCO women in non-stimulated IVF-ET program. (55th ASRM, 1999)
E. ROS(Reactive Oxygen Species)
(1) Effect of the antioxidant supplemented into semen or sperm washing medium on functional parameter of human spermatozoa (KSFS 2006)
(2) Correlation between seminal parameter of patients and sperm DNA fragmentation estimated by comet assay (KSFS 2006)
F. Stem cells
table title Adult stem cells - In vitro proliferation and differentiation of placenta derived cell and HSC isolated from umbilical cord blood
- Effect of oxygen tension and antioxidant on proliferation of HSC in vitro
mbryonic stem
cells- Establishment of gene knock-in system in hES cells
- Single cell culture of hES cells
- Differentiation of hES cells into germ cells
G. Genetics
table title Cytogenetics - Amniotic fluid
- Chorionic villi cells
- Peripheral blood / Cord blood
- Tissue
Molecular
genetics- Preimplantation genetic diagnosis (PGD, FISH)
- Preimplantation genetic screening (PGS, FISH)
- Azoospermia related gene test (Daz test)
- Amniotic fluid FISH (18, 21)